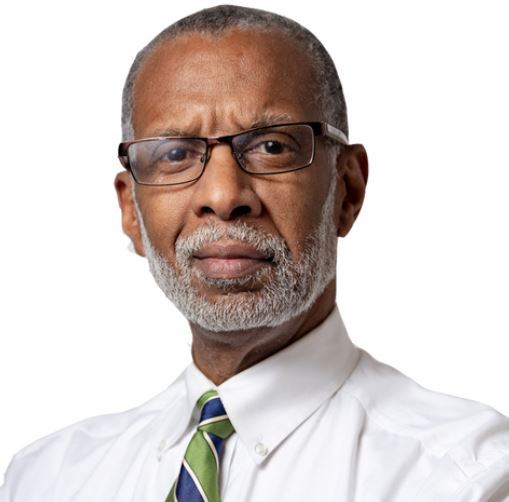
Geoff Gross, founder and CEO of Medical Guardian, has been at the forefront of providing personal emergency response and comprehensive health care engagement solutions since 2005. With 325,000 active members nationwide, including over 50,000 members here in Pennsylvania, Geoff’s fervor for connected care, age tech, and the IoT industry drives Medical Guardian’s mission: empowering members to live a life without limits.
What’s your favorite thing about working in health care?
Working in health care, I’m deeply passionate about empowering individuals to maintain their independence. It’s a personal mission for me, inspired by my grandmother Freda, who was our first member when I started the business 18 years ago. Every day, I’m reminded that we’re providing older adults the assurance they need without limiting their zest for life. It’s about being there for them, 24/7, ensuring they never have to compromise on living life their way.
What are the biggest issues facing the health care system in Philadelphia?
We’re confronting a pressing challenge: a rising population of individuals over 65 desiring to age at home, set against a shrinking pool of health and caregiving professionals. The need for innovative health care solutions to bridge this gap has never been more urgent. It’s about ensuring that this population not only receives necessary care but also maintains the quality of life they deserve. Addressing this demographic shift is crucial for the future of our health care system.
What does the future of health care in Philadelphia look like to you?
In Philadelphia’s health care future, I anticipate a critical pairing of AI and human touch. This will boost care accessibility, improve outcomes, and reduce costs. Thanks to initiatives like Governor Shapiro’s Master Plan for Older Adults, we’ll see more aging adults leveraging technology to stay at home longer and proactively manage their health.